
A microscopic view (purple)of precursor B-cell acute lymphoblastic leukemia – B-ALL. (VashiDonsk/Wikimedia Commons)
Researchers at New York’s Memorial Sloan Kettering Cancer Center say they’ve been able to successfully train a patient’s own immune cells to find and destroy cancer.
In the largest-ever clinical study of patients with an advanced form of leukemia, the researchers found that 88 percent of the subjects treated with their own genetically modified immune cells were able to achieve complete remission from the disease.
“These extraordinary results demonstrate that cell therapy is a powerful treatment for patients who have exhausted all conventional therapies,” said one of the study’s senior authors, Michel Sadelain, director of the Center for Cell Engineering at Memorial Sloan Kettering. “Our initial findings have held up in a larger cohort of patients, and we are already looking at new clinical studies to advance this novel therapeutic approach in fighting cancer.”
The study findings were reported in Science Translational Medicine.
The patients in the study all suffered from a relapse of Adult B cell acute lymphoblastic leukemia (B-ALL). This form of blood cancer develops in a person’s B cells, a type of white blood cell.
B-ALL can be difficult to treat. Most patients tend to relapse after successful initial therapies and there are few treatment options for those who do relapse.
One of the few treatment options is an aggressive form of chemotherapy called salvage chemotherapy. But, of all the relapsed B-ALL patients who have this treatment, only about 30 percent respond positively.
Even if the salvage chemotherapy is successful, the patient would, at best, be in remission and not cured.
For any hope of long term survival, B-ALL sufferers need to undergo a successful bone marrow transplant.
For the study, the team gathered 16 people with relapsed B-ALL and infused the volunteer patients with dosages of their own genetically modified T-cells, another white blood cell that protects the body from infection.
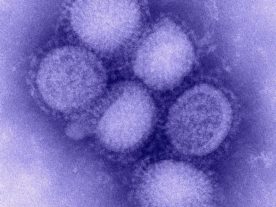
So why can’t our T-cells naturally fight cancer as they do with viruses like the flu? It turns out that our immune system isn’t able to recognize cancer cells as foreign intruders as it would with other forms of infection. So, in their natural state, T-cells aren’t helpful in attacking cancer cells.

Scanning electron micrograph of a human T lymphocyte (also called a T cell) from the immune system of a healthy donor. (NIAID via Wikimedia Commons)
Immune cells need to be specially trained to find and destroy cancer cells. The researchers “taught” the T-cells through genetic modification to look for and kill cancer cells that contain a protein called CD19.
According to the study, the successful results achieved by this form of therapy far exceeded the positive response rate of patients who had salvage chemotherapy treatment alone.
There were side effects to the cell therapy, including flu-like fever, muscle pain, low blood pressure and difficulty breathing, something the doctors referred to as cytokine release syndrome. Cytokine is a form of protein.
The study’s investigators are continuing their research to see whether cell therapy could be as successful at treating other forms of cancer as has shown to be with relapsed B-ALL.


















Is t cell research only available for the study of leukemia or is it being done on any other form of cancer?
This is just a thought. If we can alter T-cells to fight cancer could we alter T-cells to combat Aids. My idea is to modify T-cells so that they genetically resemble HIV. That way, if HIV is introduced to the body the virus would believe the host to already be infected. This would allow the modified T-cells a chance to attack the foreign host. Is it possible that those HIV cells wouldn’t respond or attack back because they believe the T-cells to be one of theirs.